Causes of Achilles BursitisInflammation of the achilles bursae and/or the achilles tendon usually develops due to overuse, trauma, or degeneration of the protective tissue in the heel and lower leg. Specific causes include: Acute Trauma - A direct blow to the back of the heel can cause injury to the retrocalcaneal bursa. In such cases, blood may leak into the bursa causing irritation, inflammation, swelling and pain. Excess Stress - Without exercise or activity, muscles can weaken and your heel no longer has the muscle support it needs to move correctly. This can cause excess load on the lower leg and heel or your weight may be distributed unevenly within your ankle joint. Uneven distribution of weight will put extra stress on some areas compared to others leading to abnormal wear and tear on the stressed areas. Athletes Who Overtrain or runners that increase their distance to quickly are at greater risk of experiencing Achilles bursitis. With over use, the Achilles bursae and tendon can become irritated and inflamed leading to thickening of the bursae lining and wearing of the tendon. Fluid builds in the bursa when it becomes irritated causing swelling of the Achilles bursa and pain at the back of the heel.  Overuse Injury (Chronic) - Excessive friction, or rubbing, on the retrocalcaneal bursa can aggravate it over time. If your run, walk or hike often, you may be at higher risk of achilles bursitis due to frequent stress and friction on the achilles bursa. This risk increases if there is anything that many cause abnormal wear and tear within the joint. Improper foot wear, tight shoes or shoes that do not fit properly can cause extra pressure and friction on the back of the heel. Over time, this pressure causes irritation of the bursae that protects the Achilles tendon causing one or both to swell and become inflamed. Pressure on the Bursa - Work and frequent activities that place repetitive pressure on the infrapatellar bursa can cause achilles bursitis. Although the bursae in your heel function as cushions to protect the tendons and other soft tissue, frequent walking or stair climbing during your work or activities often creates more stress than they can handle. The excess pressure causes the bursa to become irritated and inflamed, leading to swelling and thickening of the bursa lining. Infection (Septic Bursitis) - The closer the bursa is to the surface of the skin, the more likely the chance of infection from specific bacteria that are commonly found on the surface of the skin. This infection is known as septic bursitis and common bacteria that create this infection are known as Staphylococcus Epidermis (or Staphylococcus Aureus). This bacteria can affect the bursa if the heel is cut or scraped, allowing it to get under the skin. Symptoms of Achilles BursitisSymptoms of Achilles bursitis are often mistaken for Achilles tendinitis because of the location of the pain at the back of the heel. When you suffer from Achilles bursitis you will experience some or all of the following symptoms which are most noticeable when you begin activity after resting. 
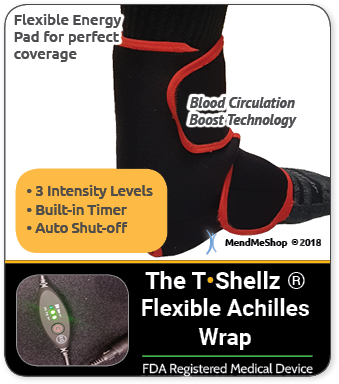
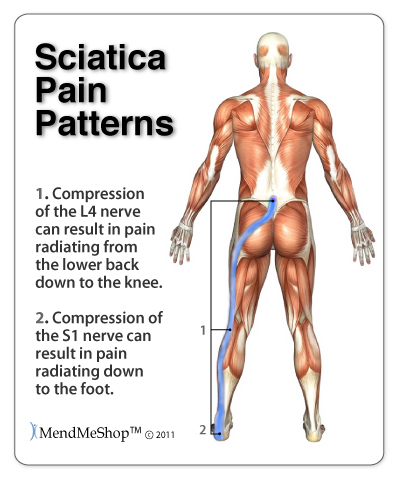
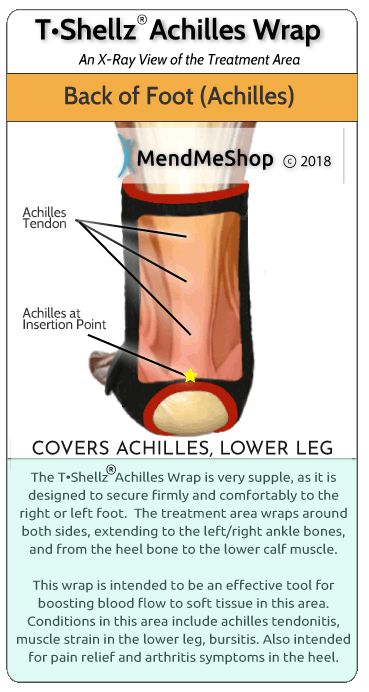
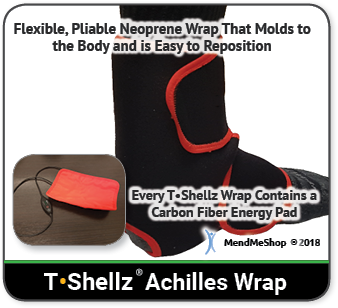
If any of those statements are true for you or you're suffering from on-going pain in your heel then you might have an injury called "retrocalcaneal bursitis". A bursa is a sac of synovial fluid, rich in protein and collagen. These fluid-filled sacs form in areas where 2 surfaces in your body - most often where a bone and tendon or a bone and muscle - rub together during movement. When pressure or friction is too high, excess fluid can build up in the bursa sac and/or the the lining of the sac can thicken, causing inflammation. When an achilles bursa becomes inflamed, moving your heel becomes painful and difficult. Any actions that put pressure on the inflamed bursa can increase irritation and cause further inflammation and pain. Bursitis occurs when a bursa is irritated from frequent pressure and it becomes inflamed. When one or both of the bursae (outlined at the top of this page) become inflamed, it is generally referred to as Achilles bursitis because of the bursa's proximity to the Achilles tendon. In some cases, an inflamed bursa can become infected with bacteria (referred to as septic bursitis) and can quickly become life threatening. It is important to see a doctor quickly if you have an infected bursa.  Achilles bursitis can happen to anyone - seriously. The achilles tendon handles extreme forces everyday, and the achilles bursae handle the friction from these forces. Achilles bursitis can happen from acute trauma (direct hit on the bursa), but often results from stress due to repetitive movements (running, walking, jogging) as part of your job or from sports related activities. Achilles bursitis becomes more prevalent due to aging as soft tissue around the ankle and bursae become weakened as we grow older. Achilles bursitis is one of those injuries that can really bring down the quality of your life. Anyone - young or old - can suffer from this injury, and if you're active this condition will keep you from doing the things you love to do. It will definitely interrupting any of your normal daily tasks and make living life harder than it really needs to be. How Do I Diagnose Achilles Bursitis?When you are experiencing heel pain and suspect you have bursitis, the best way to diagnose this condition is with a quick visit to your doctor for a physical examination of your heel. Getting a proper diagnosis is important so you can treat your condition correctly. Untreated chronic inflammation of bursitis can lead to calcification of the bursa. Calcification of the bursa will mean that it will become even more painful than before.  To begin with, your doctor will gather a medical history about you and your current condition and symptoms. He/she will ask about the amount pain you are having with your lower leg and heel. How long you have had your symptoms and if you are experiencing a range of motion loss or limp when walking/running. Details about what caused the pain in the heel, when it started, and whether or not you have ever had treatments for this or a similar condition in the past, are very helpful in assessing your injury. Range of motion movements / tests will be done to see how much movement has been lost in your heel. Your heel might hurt from the doctor poking and prodding at it, but by doing this the doctor will better understand the source of your pain, the level of tenderness in the area and how well you can move with this condition. Your doctor may also consider any previous foot/knee injuries or joint stiffness that you may have had in the past. This will help the doctor to determine if you have a more complex injury in your heel and rule out any other foot injuries that may be present. 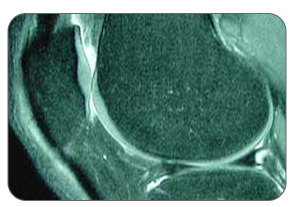 If a soft tissue injury is suspected, an MRI may be undertaken to view where and how extensive the damage in the ankle is. An x-ray may be recommended to rule out a bone spur or other foreign body as the cause of your ankle pain. Possible causes of pain that an x-ray can identify include instability, abnormal bone shapes (bone spurs or bone cysts), wear and tear on the joints, avulsion fractures (when a fragment of bone tears away from the main bone along with the muscle, tendon, or ligament as a result of trauma), dislocations, arthritis, calcium deposits in the bursa or joint, and/or other problems.  As the bursae in the heel are close to the surface of the skin, they significantly susceptible to septic bursitis (caused by a cut or scrape) than most other bursae. Your doctor may aspirate (use a needle) to remove fluid from the bursa to check for possible staphylococcus epidermis (or staphylococcus aureus) bacterial infection. Your doctor will be able to determine whether there is an infection or not by drawing a small sample of the bursa fluid with a needle. If it is determined that your bursitis is septic, you will be prescribed antibiotics to get rid of the infection. A physical examination will be performed to determine if you have any signs of Achilles Bursitis or other ankle injury. He/she will look and feel the soft tissue and bones in your ankles to note any differences between the two of them. This will identify any abnormalities, such as swelling, bone deformities, atrophied muscles, redness and/or warmth on the skin. In many cases, the first sign that you have Achilles bursitis is swelling in the back of the foot and ankle pain. As the subcutaneous bursa is close to the surface of the skin, it is more susceptible to septic, or infectious, bursitis caused by a cut or scrape at the back of the heel. Septic bursitis requires antibiotics to get rid of the infection. Your doctor will be able to determine whether there is an infection or not by drawing a small sample of the bursa fluid with a needle. Are You Sure It Is Achilles Bursitis?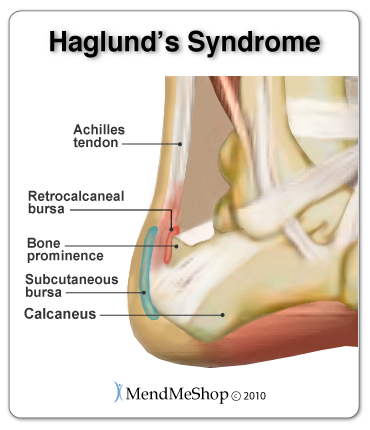 Pain, swelling and inflammation at the back of your heel could mean that you have achilles bursitis, but it's also important to consider that there are other conditions that might cause pain and swelling in the area too. Visiting your doctor when you have achilles pain is always recommended, as there are many possible issues that can happen within the Achilles and ankle. Sometimes, one set of symptoms can result in multiple diagnoses. Haglund's Deformity (also known as Haglund's Syndrome) refers to an enlarged boney protrusion on the upper, back part of the heel bone. It is caused by calcification of the heel bone due to the inflammation of Haglund's Syndrome, a combination of Achilles tendinitis and Achilles bursitis. The boney protrusion causes further irritation to the retrocalcaneal bursa and Achilles tendon as it presses them between the protrusion and your shoes. This increased irritation then causes Haglund's Syndrome to become worse. Due to similar symptoms and the location in the Achilles tendon area, Haglund's Syndrome is frequently misdiagnosed as Achilles tendonitis. 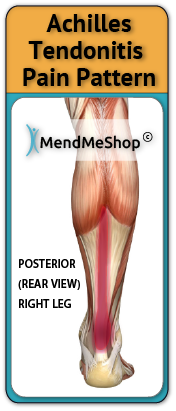 Achilles Tendon Strain If you have a strained achilles tendon, you will experience pain along the back of your foot and above your heel, especially when stretching your ankle or standing on your toes. Most strains are mild, though this condition can persist and worsen if conservative treatment methods are not undertaken. The seriousness of the strain will most like affect the way you walk, forcing you to limp due to pain. A sudden increase in your activity or improper warm ups before activity can cause an Achilles tendon strain. Trying to go fast, jumping (hurdles), cutting (football) or twisting in the air are just some of the scenarios with an advanced risk of developing achilles tendon strain. Achilles Tendonitis Achilles tendons carry our entire body weight so it makes sense that the achilles tendon is the thickest, strongest and most powerful tendon in the body. The achilles tendon responsible for many things, allowing you to walk, run, jump, or stand on your toes. Due to the major stresses taken on by this tendon, it is often injured either. Injury can also be attributed to overuse or as a result from excessive strain (even a traumatic accident or sudden pop). If you have tendinitis of the achilles, you will be suffering from irritation and inflammation in the back of the foot - just above the heel. Tendonitis is a result of degenerative tears within the tendon itself, and these microscopic tears are much akin to a rope that is starting to fray from excessive load. Achilles Movement and the Re-Injury CycleEvery time you flex your ankle, those ligaments and muscle tissue move; when they are inflamed, every movement hurts. Once this tissue is injured it's painful and becomes very difficult to recover 100% without proper treatment. Re-Injury of the Achilles Tendon Must Be Avoided At All CostsConstant re-injury needs to be avoided at all costs! Please excuse the obvious statement, but I really need to drive this point home. Re-Injury is very common... why? Everyone wants to get back to their regular lifestyle once the pain has reduced. Here is where you have to be careful - often, much of the pain is due to inflammation - so, once you iced the area and the swelling dropped, a lot of the pain probably disappeared too. So then you start back at your regular lifestyle and then all of a sudden the old injury starts flaring up again - this is re-injury! The Pain May Have Dropped But It Does Not Mean The Underlying Injury Has HealedRe-Injury is bad because sure, it delays the healing process, but what's worse is that every re-injury and additional healing cycle increases the amount of scar tissue that builds up in the area of your original achilles injury. This applies to muscle, tendons, ligaments and other connective tissue as well. Scar tissue is a weak form of collagen - hard, inflexible, and tough to get rid of once it begins to take hold. The more scar tissue that develops, the more you lose the range of motion in your ankle. With excess scar tissue build up, the injured tissues and the achilles in general will remain weak and very prone to re-straining and re-tearing. While you can go a number of days and even a few weeks without any major setbacks during the injury.. inevitably, a certain movement or motion will happen that causes your injured soft tissue to strain and even tear once again. This is attributed to the scar tissue build up and will result in the buildup of yet more scar tissue and a further reduced range of motion (ROM). The more scar tissue that develops, the greater the risk of winding up permanently injured with chronic pain or arthritis. Scar tissue means that your achilles will not perform as well as it once did and it makes it much more prone to injury later on. The longer the injury remains, the risk of atrophy increases and the risk of more scar tissue increases. This is why it is critical to treat your achilles injury now rather than later. 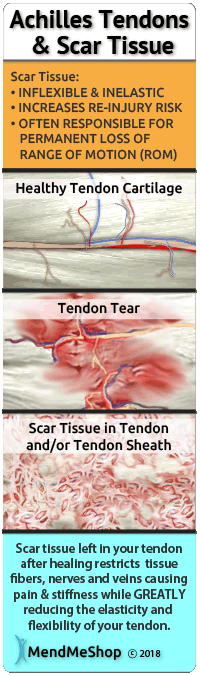 Continuous re-injury and build-up of scar tissue makes it more likely that you will wind up with chronic pain, reduced Range of Motion or even arthritis (permanent damage).An Achilles Injury Does Not Have to Persist For Months Or Longer. Here is Why It Does For ManyRecovery from an achilles injury can take a long time, especially when some of the less effective, traditional methods are utilized. This is simply because many treatments either focus on masking of pain or are too inconsistent to provide sustainable improvement. 1: Bursitis Sufferers Continue to Aggravate & Re-Injure Their BursaIt goes without saying that anyone suffering from bursitis should want to minimize their chance of worsening the injury, or re-injuring the bursa once it has started to get better. Obviously, a worsening injury will delay the healing process, but what's worse is that every re-injury and additional healing cycle increases the amount of time that your joint is immobilized. Time is not kind to an immobilized joint - you lose strength in the joint but worse than that, you lose the range of motion in your joint via atrophy (your flexible tendons, muscles and ligaments slowly shrink, decreasing joint elasticity). The more time that goes by with an immobile joint, the more likely you will wind up with a chronic joint problem (long term injury such as tendonitis or persistent bursitis pain). Basically it means that your joint will not perform as well as it once did and it becomes more prone to injury again later on. If you have an inflamed bursa in one of your joints, it's very important to heal it quickly and completely. Minimizing the healing time of your bursitis should be an obvious goal, as bursitis typically limits your ability to go about your daily routine. As stated here (MedicineNet.com), if your long-term (chronic) bursitis is left untreated, calcium deposits can form within the bursae. These calcium deposits can lead to permanent stiffness in the affected joint. 2: Visits to Physio (PT) Help - We Always Recommend It - But It Can Be Costly And InconvenientWhile the benefits of PT are very real and we believe it to be integral for recovery from soft tissue injuries, the problem is that people only attend sessions a few times a week. To truly provide a long term solution to combat bursitis induced soft tissue damage, you need to be receiving multiple treatments on a daily basis and get rid of your bursitis asap. Not just any type of treatments, but ones that focus on generation of new healthy tissue - along with proper synthesis of that tissue as well. Treatments for soft tissue injuries are cumulative in nature...meaning the more the treatments are administered, the faster the benefits can be experienced. Who these days has time to visit a clinic on a daily basis? Not only is your time limited, but the cost of daily PT sessions is out of reach for most people. Therefore, the focus needs to be on adding treatment options that can be done frequently, from the comfort of your own home (and even the workplace if the opportunity presents itself). We will discuss these options later on down the page. 3: People Tend To Focus Too Much On Cold TreatmentsThis is the final reason for extended bursitis and soft tissue injuries. We see it all the time - people for weeks and even months only focus on using cold. Doing too much cold will actually inhibit the recovery because you are starving the injured tissues of the blood flow they need to repair and rebuild the collagen. Cold restricts the vessels - reducing the blood flow to the tissues that truly need it most. Cold treatments should be more focused on in the earliest stages of an injury with much less focus in the mid and latter stages.The truth is, there will always some mild inflammation associated with tissue injuries. However, some of that inflammation will remain UNTIL you begin to focus on healing the soft tissue (muscle). Once this begins to heal, the inflammation will then subside more permanently - not just temporarily like with cold treatments. As an analogy, think of a home with a leaky roof. You can place a bucket on the floor of the attic whenever it rains - and this will help temporarily, but does it truly address the situation? Obviously the answer is no. Not until you focus on repairing the structural issues with the roof - will the problem be actually solved. The same concept applies to injured soft tissue - you need to focus on reinforcing growth of flexible, strong tissue. To do this, you need more blood flow reaching them, not less. 4: Injections Can Cause Harm If You Are Not CarefulThis can be VERY helpful in alleviating pain and when it comes to bursitis, pain relief alone can make a huge difference. However, some people get a false sense that their injury is healed because they are not experiencing the pain they once did. Some individuals even engage in activities they should not be doing because they "no longer feel pain". Once the effects wear off, people often find their bursitis persists . This of course, results in a prolonged recovery. Be very careful about your activity after the injection because there is little, if any, pain feedback to tell you that you're overdoing it. Merely masking the pain can be very helpful temporarily, but it is not a solution; it is just a temporary fix. Achilles Injuries Not Only Affect the Achilles - But Can Lead to Other Conditions and Injuries. Every time we use our injured heel, damaged and swollen tendons and muscle tissue move; when they are inflamed, every movement hurts. With injured tissue, pain happens - sometimes a LOT of pain, so we try not to move it. So, when doing something we need to use our heel for (getting dressed, driving, talking on the phone), we start to use the knee and even the hips more. If we can, we use our other foot instead, even though it is inconvenient and usually the non-dominant foot. A couple days later (after purposefully avoiding movement of our achilles), the pain has gone down (as well as the swelling) and this is where the trouble begins! The pain disappeared with the swelling but we still aren't fully healed! Not knowing this, we start using our achilles normally again and then the pain shows up again like it did before - all because the injury wasn't fully healed in the first place. Eventually, we use the other joints more and more, instead of having to put the injured achilles under strain again. This is why these other areas start to hurt - they are being overused now. Soon, aches and pain can become commonplace in other areas of the lower body - all as a result of the original injury and the body's instinctive nature to "protect" the original achilles tendon injury - all because the injury wasn't fully healed in the first place! We continually re-injure the achilles through our daily activities and now this injury has become a chronic achilles injury. Muscle imbalances result, placing tension on bone and softer tissues - leading to a misalignment within the lower body. The extra stress on the opposite side of the body will also result in weakness and fatigue of the tissues - increasing the chances they can eventually be injured or gradually degenerate. This is a textbook example of how you get an overcompensation injury. In some cases, physical therapists warn that overcompensation can be very dangerous as it will eventually affect gait or alignment on a permanent basis. An injury to one achilles can easily lead to straining in other areas, making an overall recovery hard to initiate. The longer the injury (and corresponding pain) persists, the greater the chance that you will sustain more strain from overcompensation, eventually leading to issues in those areas as well. To minimize potential secondary injuries, know that it is important to deal with your achilles heel tendon injury quickly and completely. Truly, chronic achilles/calcaneal tendon and bursa injuries can become a vicious cycle - which is why it is absolutely critical to focus on methods that improve and strengthen injured soft tissue in a timely manner. The faster you truly heal, the less chance you have of sinking into a downward spiral of re-injury, scar tissue growth and overcompensation injuries. Okay, So I Have Achilles Bursitis...What Should I Do Now?If you want to dig deeper into home treatment options, view our Bursitis Treatment Page Here Surgery, Post-Surgery Rehabilitation and Achilles Tendon ExercisesIf you have undergone surgery or your achilles (reattachment, repair or graft) and are looking for rehabilitation information, click here. Increasing flexibility and strength in the ankle is a key component to speed healing and avoid re-injury. For this reason, we have created ebooks that outline specific exercises / stretches for our clients undergoing achilles injury recovery. Even when you're injured and in pain you need to keep moving to break-up scar tissue that's forming in your tendons and ligaments in your ankle and calf. Regular movement can increase healthy range of motion (ROM) of your ankle, guaranteeing you a speedier recovery process and return to regular activities. Moving when you're injured is hard. Since moving while injured can be painful most people think it's better to stop moving, rest their foot and hope that their achilles injury will heal all on its' own. Even though rest is important to recovery, too much rest during the recovery process will increase the amount of scar tissue in your lower leg. Circulatory Boost treatments combined with a proper stretching regimen will help decrease scar tissue growth while increasing elasticity and strength in the lower leg and ankle joint. During the healing process your body will fill in soft tissue tears with dense, brittle tissue called "scar tissue". The human body will use scar tissue as a temporary solution and will try to build the scar tissue as fast as possible to heal a tears in the soft tissue. Scar tissue can form fast to bring together the edges of a tear, but working fast doesn't mean that the job's done right. When scar tissue forms it doesn't come together as neatly as regular (healthy) tendon/ligament tissue would. Scar tissue fibers will lay down over top of your tear in a cluttered, messy and jumbled up way. Ankle Joint Atrophy is arguably a bigger issue than scar tissue. Whether you have a ankle/lower leg injury or have recently had an operation in that area, you will find that the joint has a more limited range of motion than you had before. In most cases, this is due to atrophy - the shortening of connective tissue in the lower leg, knee and ankle due to inactivity. In cases where atrophy exists, it is very important to stretch and do gentle exercise to nip this problem in the bud before it becomes a chronic (long-lasting) issue. If you are currently recovering from a Achilles injury speak with your physician about stretches and exercise. When done properly under recommendation of a physician, stretches have a proven track record of assisting in the speedy recovery of many patients. This is without doubt, the final essential tool for complete achilles/ankle injury recovery. Once a patient deals with the swelling and inflammation through use of a Cold Compress or Ice Pack, then begins the Circulatory Boost process by using home treatment with the TShellz Wrap, all the while keeping rested to keep stress off the injury. Once the injury has healed, it is time to take the third and final step to recovery by beginning a rehabilitation stretching regimen. Before making the transition to crutches, PTs prescribe gentle stretching of an injured achilles, especially if your are recovering from achilles reattachment surgery. They don't prescribe this to annoy you - it is in fact the most important part of injury recovery. You probably know of someone that chose not to do these stretches as it is common - and they paid a high price for it. By choosing to ignore recovery recommendations (ie. not stretching), there is a substantial risk of re-injury or even sustaining an injury greater than the original injury ever was. Consistent stretching (as prescribed by your physician or PT) not only helps minimize the growth of scar tissue, but it also increases the elasticity and strength of the achilles tendon and interconnected soft tissue. Stretching, when used in conjunction with the Achilles TShellz Wrap will allow you to be better prepared to handle higher and higher loads. Eventually you will reach a stage where your tendon can handle standing or walking for longer and longer periods of time. This is the final stage of recovery and depending on age, the nature of the injury, your weight and many other factors, it can take the longest time to complete. But remember, for achilles injuries, it pays to be patient! Rushing your tendon injury recovery almost never pays. If you do wind up getting surgery, know that rehabilitation at-home while attending regular PT or doctor appointments is vital for your overall recovery. Consistent exercise and conservative treatment on a daily basis during your rehabilitation while working with your doctor or physical therapist is key. This is why you should seriously consider maximizing your recovery by using the TShellz Wrap® at home once you are approved for PT. The more consistent you work at enhancing blood flow to surgically repaired soft tissue, the more consistent the healing process will be. Nourishing the tissues will more oxygen and nutrients (which are carried through the blood stream) will give the body a better ability to produce new, healthy collagen. In effect, you will help the body produce stronger tissues while potentially reducing the number of setbacks that can occur following surgical procedures. Click HERE to Go To Our Online Store We take all major credit cards and Paypal. Conservative Treatment Tools Our Clients Have Used to Help |
     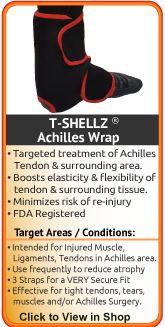   |